When camps receive negative COVID-19 screening tests, it is a result of deliberate planning, excellent communication, earned compliance, diligent execution — and a little luck! The situation of achieving negative tests is reflective of the multiple layers of nonpharmaceutical interventions (NPIs) your camp has employed and program changes that come as a benefit of these layers. Camps with lower degrees of protective layers are at greater risk of COVID-19 transmission. Many camps ask what can be changed or loosened in their programs after negative testing. Can they remove masks? Can they stop cohorting? Do they still have to encourage physical distancing?
Points to Consider
A major consideration prior to changing policies is the degree of migration in and out of camp-— especially by those unvaccinated to COVID-19 or those persons engaging in high-risk activities regardless of vaccination status. Why? These individuals are the most likely in your community to bring COVID-19 into camp. Day camps by definition have migration in and out of camp and, as such, should be wary of loosening other NPIs such as cohorting, distancing, and masking. Camps can lower the risk of migration in and out of camp by insisting that all staff regardless of immunization status do only low-risk activities when off camp, such as those that can be done masked and distanced, and only remove masks when outdoors (i.e., eating). Overnight camps can further minimize their migration risk by keeping unvaccinated or partially vaccinated staff on camp or taken off camp through supervised low-risk activities. Vaccination continues to protect against circulating COVID-19 strains, but as the delta variant becomes the dominant strain, its “hyper-transmissibility” is of particular worry for non-fully vaccinated individuals who go off camp or for day camps. If non- or partially vaccinated persons must leave or have high-risk exposures, camps should be careful to minimize their exposure to your unvaccinated campers and consider a screening testing cadence for these individuals. Day camps, especially in areas of higher COVID-19 transmission, should consider screening testing akin to the testing programs of many schools with regular weekly or biweekly screening testing.
Another consideration is that if we remove our masks and expand our cohorts, many other viruses will take advantage. Many camps have already experienced the rise in non-COVID-19 colds and strep throat triggering isolation and COVID-19 testing. Your camp health center needs to be prepared to evaluate and manage symptoms as they arise and be able to ensure that the symptoms are not COVID-19, if necessary. The NPIs of masking, distancing, hand hygiene, daily health screenings, early identification, and isolation help keep respiratory illnesses, not just COVID-19, at bay.
If you have protected your camp “bubble” and have negative post-arrival screening tests, what now? First and foremost, camps should adhere to their state and local public health guidance. If allowable, camps could consider collapsing smaller cohorts into larger ones that allow for expanded programming opportunities. Could your bunks be made into an age group cohort? Could vaccine-eligible age groups with higher vaccination rates be made a single cohort? Maintaining firewalls between cohorts decreases risk of infectious spread across cohorts if COVID-19 (or other viral illnesses) spreads. Therefore, if considering expanding cohorts, consider enhancing other NPIs (handwashing, ventilation, screening) to help minimize spread of respiratory illnesses.
What changes could be considered in your masking policies?
The federal Centers for Disease Control and Prevention (CDC) camp guidance recommends masking indoors for unvaccinated persons and masking outdoors for unvaccinated persons if in an area of high transmission where distancing cannot be done. Additional guidance about cohorts indicates that they are living units of permissible maskless/non-distanced interaction. What are the impacts for face masks if you decide to collapse or change your cohorts? Consider the implications for not only COVID-19 but transmission of other respiratory conditions. Your local and state public health guidance may have different instructions; therefore, be sure to follow their requirements.
However, when camps have done due diligence as mentioned above and have negative tests from all in the community, they might consider allowing campers and staff to not wear a mask when outdoors, regardless of vaccination status. While the transmission rate of COVID-19 is lower outside, camps must know that the definition of prolonged contact remains the same whether indoors or outdoors. We know that COVID-19 and other respiratory diseases spread more easily indoors, and camps are strongly advised to maintain masking for unvaccinated persons in this setting, particularly if multiple cohorts are using a crowded indoor space. The decision to not mask indoors or outdoors after testing essentially results in a single cohort for camp. If camps choose this route, they must consider their capacity related to contact tracing, isolation, and quarantine, and what it would mean for their camp in terms of numbers, severity of infected individuals, facilities, and end of the program.
Camps must balance multiple concepts when making the decision to not mask:
- The exceedingly low risk of COVID-19 in camp after a lengthy and diligent multi-layered NPI approach including testing, time, and migration in and out of camp
- The desire and/or need of the camp program to allow unmasked activities
- The impact of contact tracing, isolation, and quarantine capacity should COVID-19 occur
- The use of other NPIs that are in place to address transmission risks
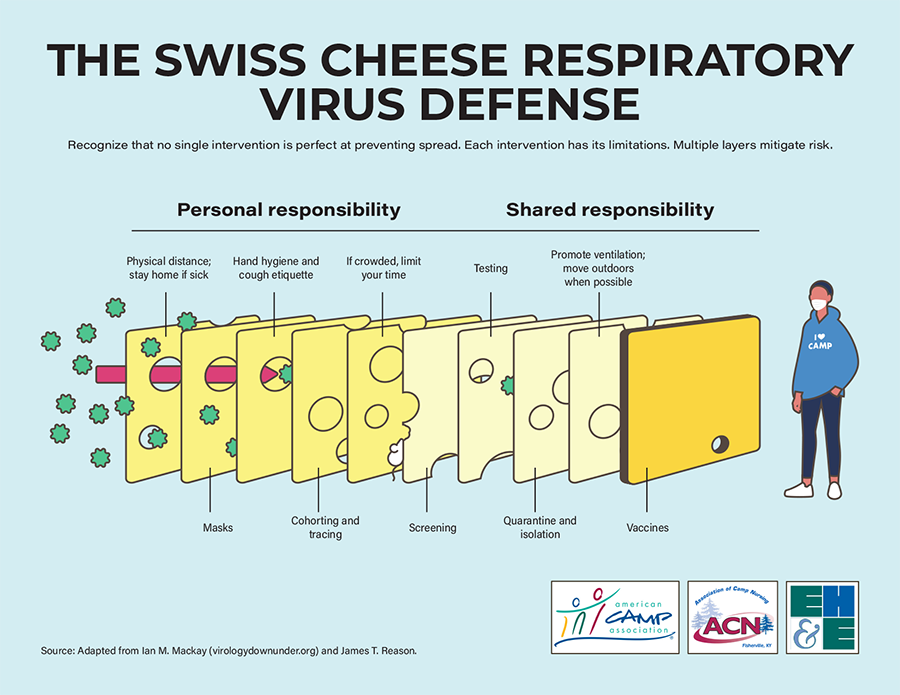
Determining your camp's path forward may look different or nuanced from other camps. Ultimately, camps must balance tolerance for small, but real and non-zero risks, with the unique and individual needs of our camp programs. As we each decide on our goals for the summer, most of us would include “no COVID-19” in that list. How the diverse and creative camp community works toward layering NPIs to achieve that goal will look different — yet we must learn from prior outbreaks that negative tests alone may not sufficiently help us meet that goal.
Infographic: Swiss Cheese Respiratory Virus Defense
The views and opinions expressed by contributors are their own and do not necessarily reflect the views of the American Camp Association or ACA employees.



